Overcome: Reducing ICU patients’ anxiety through medical alarms feedback provision
Oct 2019 - ongoing
Introduction
In the Intensive care units (ICUs), sounds (e.g., medical alarms) act as stressors that affect patients’ physiological and psychological well-being. Therefore, the stress that sounds provoke might lead to a range of psychological discomfort raging from anxiety and delirium in the ICU or post-traumatic stress disorders (PTSD) after discharge. In light of the issues, I studied the ICU patients’ medical alarms experience focusing on the interactions between alarms, patients and nurses.
Medical alarms are stressors for patients – especially – since their ambiguity and the lack of control. They are designed to alert clinicians regarding a variation on a patient’s predetermined normal status, and intended as a tool that help medical staff to improve the safety of their patients by communicating information that requires a response or awareness (Branson et al., 2008). Alarms may follow a hierarchical order in some medical devices, such as crisis alarm (detection of life-threatening situations), system failure (detection of life-threatening device malfunction), warning alarm (detection of imminent danger), system warning (detection of potential device malfunction), advisory alarm (detection of unsafe situation) (Branson et al., 2008), and their interpretation require a trained staff. Unfortunately, and mainly due to false alarms and alarm fatigue, even trained staff can lack on providing patients with proper support when a medical alarm goes off. It has been shown that reaction time of a healthcare professional, on average, can range from a minimum of 20 seconds to a maximum of 5 minutes before reacting to an alarm (Bridi et al., 2014) meaning that patients can be exposed to such a stressor longer than expected.
Patients who lack knowledge and control over the alarms are oblivious of their meanings and left to submit to the stressor while waiting for the arrival of a nurse. Nurses are resource persons who have the information to convey to patients which are needed by the latter to reduce their uncertainties and stress (Peplau, 1997).
The knowledge gained by studying the context and the issues related to medical alarms helped me to understand the patients’ constraints and needs, as well as the challenges both patients and nurses face when a medical alarm goes off. By doing so, I developed a solution that can reduce the anxiety levels of ICU patients when an alarm goes off – the so-called Overcome.
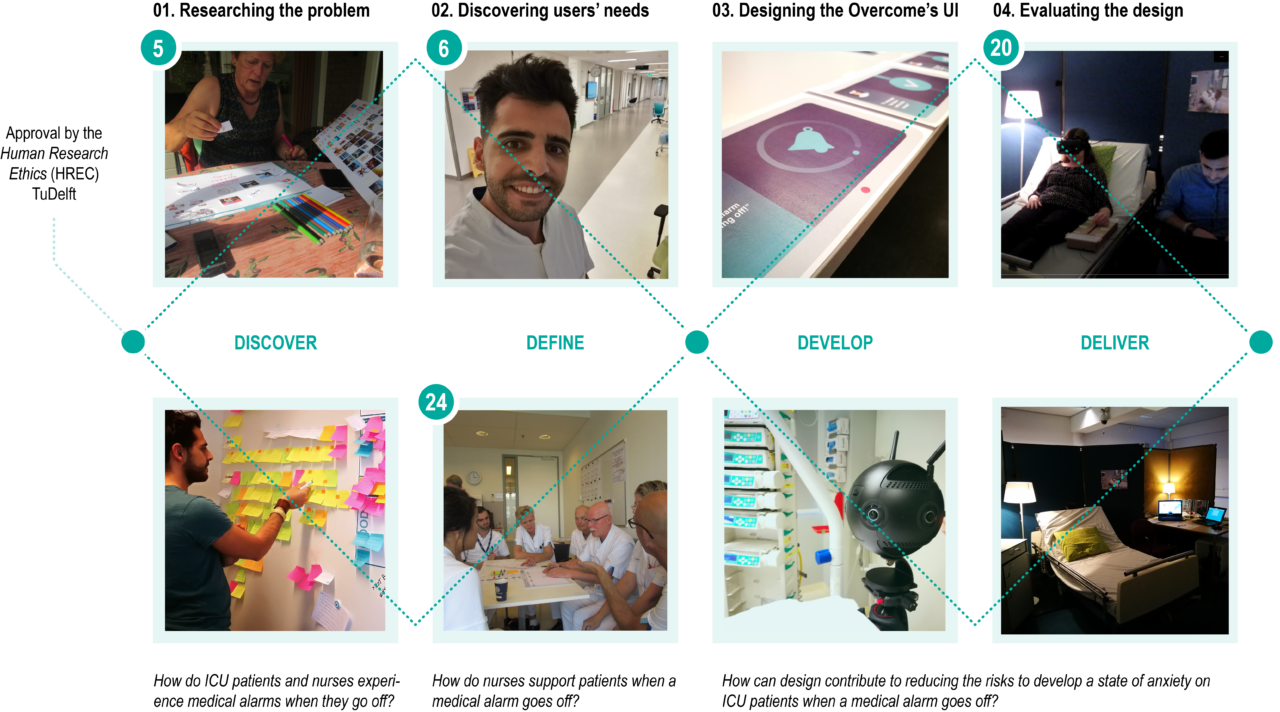
Methods
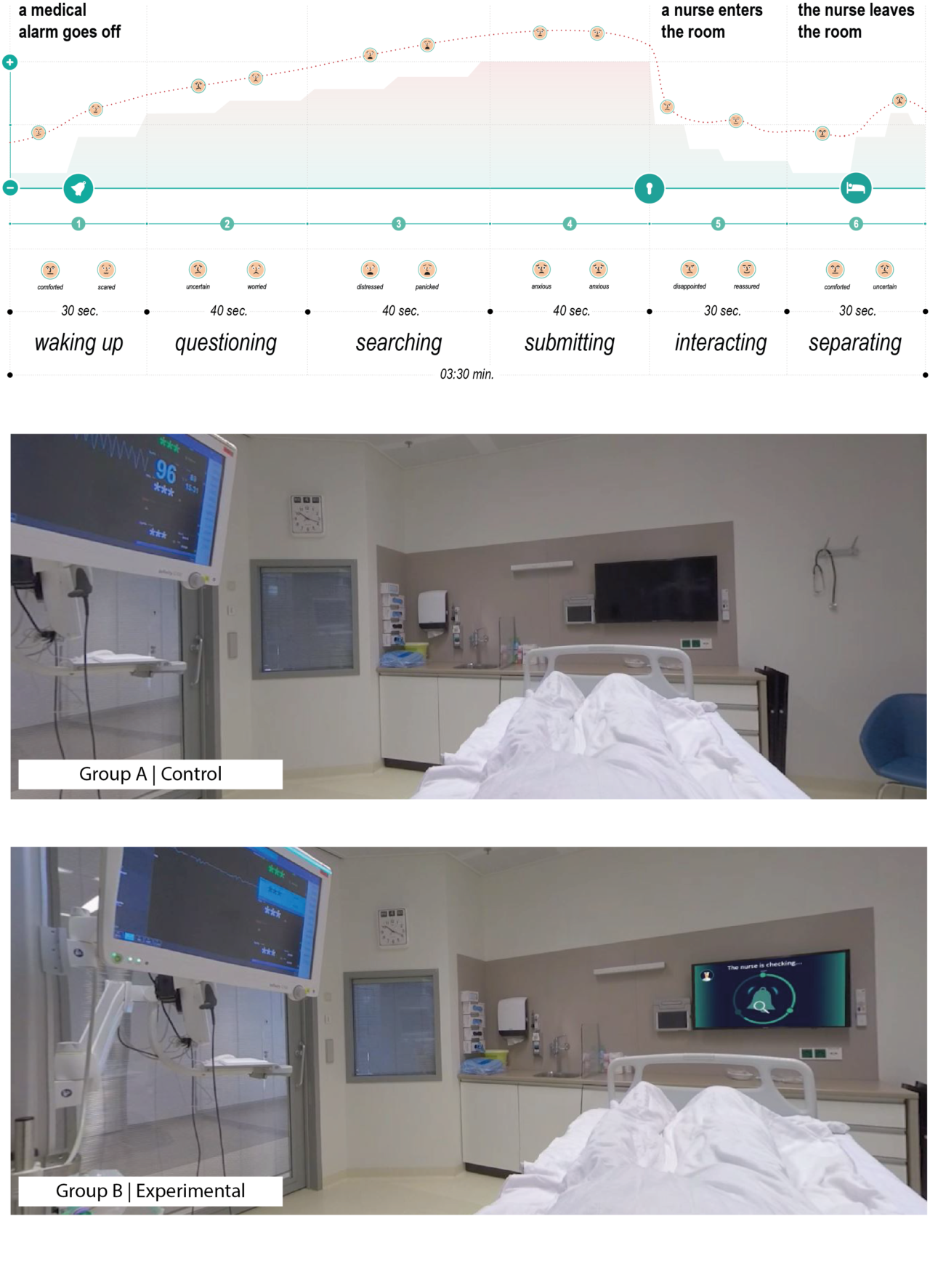
The first aim of the assignment, understanding and defining the ICU patients’ medical alarms experience including their interactions with alarms and nurses, was addressed through Contextmapping. Observations, interviews and co-creation sessions with ICU nurses and former patients created a rich dataset that was essential to deeply understand the users experience and define phases, issues and challenges both users face. Finally, I evaluated my design by using Virtual reality as an experimental setup showing that people using Overcome experience lower level of anxiety compared to those who did not.
ICU patients’ medical alarms experience
Lack of resources limit the patients’ possibilities to cope with a medical alarm. According to former patients, medical alarms are perceived as a threat and appraised as dangerous (despite their real meaning).
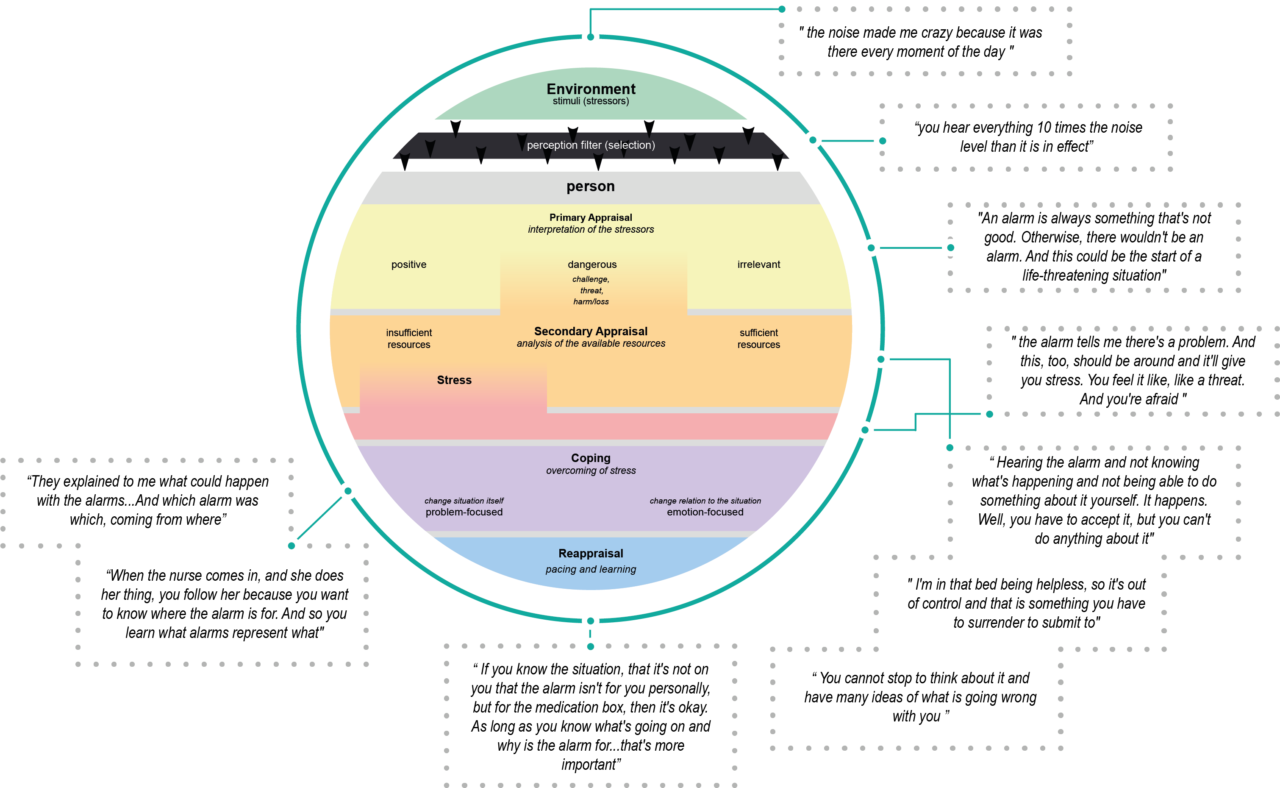
The research conducted together with former patients led me to define eight phases of the ICU patients’ medical alarms experience. These phases are described with respect to patients’ experienced emotions and patient-nurse interactions. The experience starts from the moment when a medical alarm goes off to the moment when a nurse leaves the room.
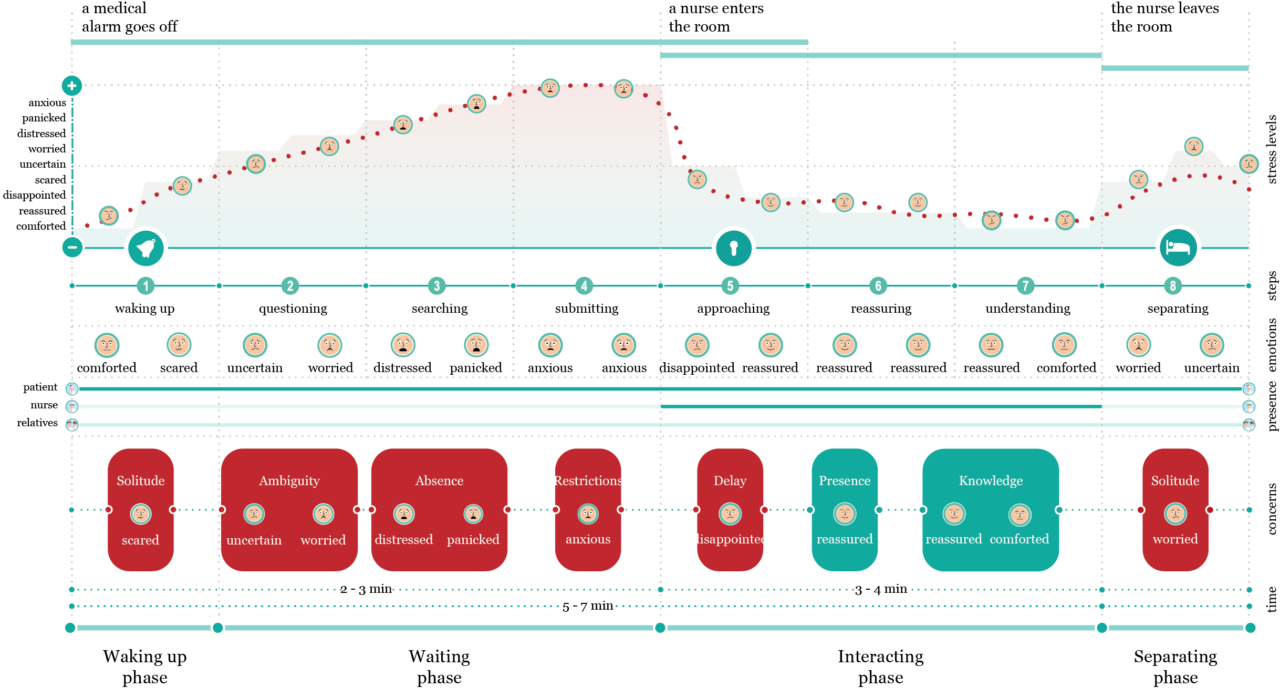
The longer is the waiting time for the arrival of a nurse, the lower is the patients’ perception of being in a safe situation. The ambiguity of a medical alarm and long waiting lead patients to the uncertainty of dying. Waiting reduces the patients’ hope of being rescued because the longer is the waiting, the less are for them the chances to reduce the risks to die. Therefore, when waiting longer than expected, patients start to doubt the fact that nurses are aware of the ongoing alarm. The most interesting event in this map is that the patients’ anxiety levels reduce only after a nurse enters the room.
Overcome
How to restore the patients’ perceived sense of safety when a medical alarm goes off and the nurse is unable to communicate with them?
By investigating on the interpersonal relationship between patients and nurses and on the way how they interact when a medical alarm goes off, it was possible to identify five different levels of information: Level of acknowledging, Level of informing, Level of instructing, Level of comforting and Level of distracting. These levels not only represent the structure of Overcome in terms of content shown but also the strategy applied by nurses to calm patients down.
Overcome is a digital interface that facilitates patients’ understanding of medical alarms and inform about nurses’ decisions towards an alarm through the provision of visual feedback.

Overcome acknowledges patients about an alarm by showing that a nurse has received and visualized the notification reporting an ongoing alarm (Level of acknowledging). In the next step, Overcome shows patients that a nurse is taking care of the situation by checking on the reason for the ongoing alarm and, consequently, a message explaining the meaning of the alarm is shown (Level of informing). In the next step, patients are instructed by a distance from a nurse on how to solve the alarm; such information is given only in case of false alarms since, in case of life-threatening alarms, nurses directly reach a patient’s room (Level of instructing). In Overcome, the level of comforting was accomplished by sharing with the patient information about the time needed by a nurse to arrive in the room. Finally, the level of distracting consists of the capacity of the interface in capturing the attention of the patient while waiting for a nurse and moving his/her focus away from the auditory stimuli.

Evaluating the concept
Testing Overcome with real ICU patients and at the ICU required permission from a Medical Ethical Committee. Due to the time restrictions, it was necessary to think about an alternative method for testing the impact of the Overcome on reducing anxiety. As a result, we decided to use Virtual Reality (VR) as experimental setup to evaluate the concept.
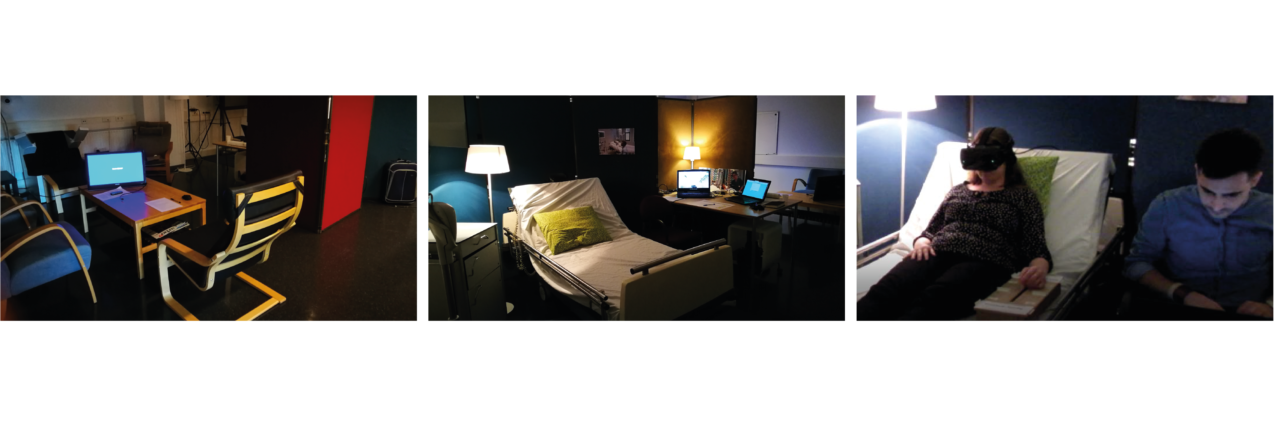
A collaboration between the Critical Alarms Lab, the VR Zone Lab (TU Delft) and the Erasmus Medical Center (EMC) gave me the possibility to create a VR experience which consists of a video made with a 360-Degree Spherical Virtual Reality Camera in an ICU room at the EMC. The video shows an ICU room from the perspective of a patient. Subjects who participated to the experiment were able to experience the phases patients go through when a medical alarm goes off. A Between-groups design experiment was performed in a three-day study period to compare the physiological reactions and subjective evaluations of anxiety in relation to the proposed experience between an experimental group (Group B) – who interacted with Overcome (variable tested), and a control group (Group A). Therefore, only participants from the experimental group were asked to evaluate Overcome feedback interface on usability, provision of information and design qualities.
Data on physiological reactions were based on Heart Rate variability (HRv) readings and collected by means of a chest strap connected via Bluetooth to an application (Elite HRV) that was recording the HRv values. Data on subjective experience of anxiety were collected by means of a Slider device and the State-Anxiety scale. Participants were asked to interact with the slider device during the experience and determine their level of anxiety by moving the slider from 1 (Not anxious at all) to 10 (Really anxious); on the other hand, the State-Anxiety scale, a subscale of the State-Trait Anxiety Inventory (STAI), was used to determine – in a more objective way – the participants’ level of anxiety two times, before and after the experience.

By comparing the data gathered from the two groups through the three different anxiety measurements methods, we showed that the State- Anxiety Scale revealed that exists statistical evidence that Overcome has an effect on reducing people state of anxiety.
Graduation Report
References
Branson, R., Eichhorn, J., Frantz, I., Mininni Rn, N., Msee, F. O., & Verklan, M. T. (2008). Advisory Board Continuing Education for Nurses (CE) and Respiratory Therapists (CRCE).
Bridi, A. C., Da Silva, R. C. L., De Farias, C. C. P., Franco, A. S., & De Lima Quintas Dos Santos, V. (2014). Tempo estímulo-resposta da equipe de saúde aos alarmes de monitorização na terapia intensiva: Implicações para a segurança do paciente grave. Revista Brasileira de Terapia Intensiva, 26(1), 28–35. https://doi.org/10.5935/0103-507X.20140005
Peplau, H. E. (1997). Peplau’s Theory of Interpersonal Relations. Nursing Science Quarterly, 10:4, 162–167.